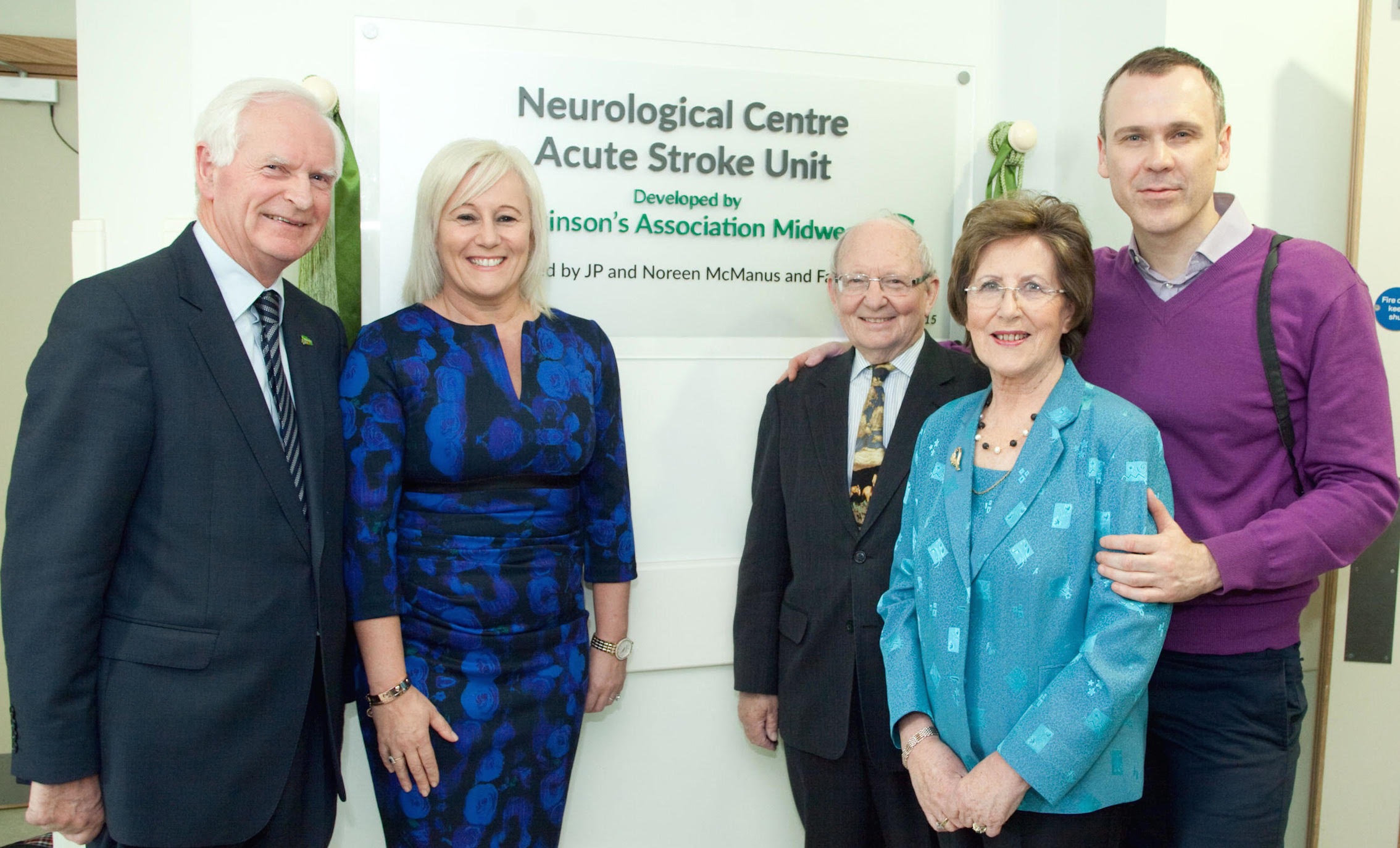
Leben Building Neurological Centre Acute Stroke Unit at University Hospital Limerick
A new era in the care of Parkinson’s patients at University Hospital Limerick has been marked with a ceremony this Friday at the newly opened Leben Building Neurological Centre/Acute Stroke Unit. A plaque has been unveiled in recognition of the contribution of the Parkinsons Association of Ireland MidWest Branch in developing the unit and the … Read more